No such thing as not disabled enough
October 3, 2022
I have never been the picture of health. From a young age, I struggled with feeling fatigued, weak, achy and dizzy. I was passed from provider to provider because something wasn’t quite right. At first, doctors suggested it was just growing pains, yet my symptoms persisted and eventually worsened. I lost weight, I lost energy and eventually I lost interest in the things I enjoyed. Classes, activities and even friendships became a chore.
After searching for answers for almost a decade, in my junior year of high school I was diagnosed with dysautonomia, a broad term encompassing over 15 specific conditions that affect the body’s ability to regulate its involuntary responses, like heart rate, blood pressure, body temperature and digestion. Patients may experience fainting spells, digestive tract paralysis, heart problems, fatigue and migraines. Dysautonomia can make it hard to walk a few hundred feet.
Despite being a disabling condition, its symptoms are often not apparent, leading to the assumption that patients exaggerate or fake symptoms. I consistently found that teachers, peers, community members and even medical professionals just did not understand. People told me it was all in my head more often than they offered to help manage my symptoms or improve my quality of life. It took me nearly a year to get a steady 504 plan, partially because it was a rarity at my high school but also because my teachers and administrators couldn’t quite comprehend the need for one because I didn’t fit their conception of someone with a disability.
Much of the discrimination that I faced didn’t come from malfeasance but rather a lack of education. I can understand this because I too used to think the same way. Prior to developing my own, I thought of disability as mobility aids, hearing aids and other things that indicate visible physical impairments, but those only account for a very small percentage of disabilities. The exclusion of non-apparent disabilities, including mental illnesses and other chronic illnesses, perpetuates the stereotype that disabilities have to be visible and discredits the experience of many people living with various types of disabilities.
Realizing that my experience didn’t stem from intentional discrimination, but rather misconceptions, made me want to educate people and share my personal experience. However, I felt it was too much to take on by myself. Additionally, I internalized stereotypes about what disability should look like and questioned whether I was even qualified to speak on the topic. I found myself disabled by my condition and craved support from people who understood what I was experiencing, but I felt like I wasn’t disabled enough and didn’t truly belong in the disabled community. After struggling for years with my identity, I realized that I deserve the same amount of support and respect as any other disabled or able-bodied person, and I wish that I had someone to teach me that sooner.
Realizing that my experience didn’t stem from intentional discrimination, but rather misconceptions, made me want to educate people and share my personal experience.
I realized that I needed to speak up because not being believed or taken seriously was emotionally exhausting, and I didn’t want anyone else to have to live with that exhaustion because they didn’t feel like they were disabled enough.
One of the most integral parts of embracing my disability was seeing other patient advocates share their stories. Through these communities, I finally found somewhere I belonged and people that genuinely understood me. My experiences qualify me to speak on the topic, and there’s no such thing as not being disabled enough.
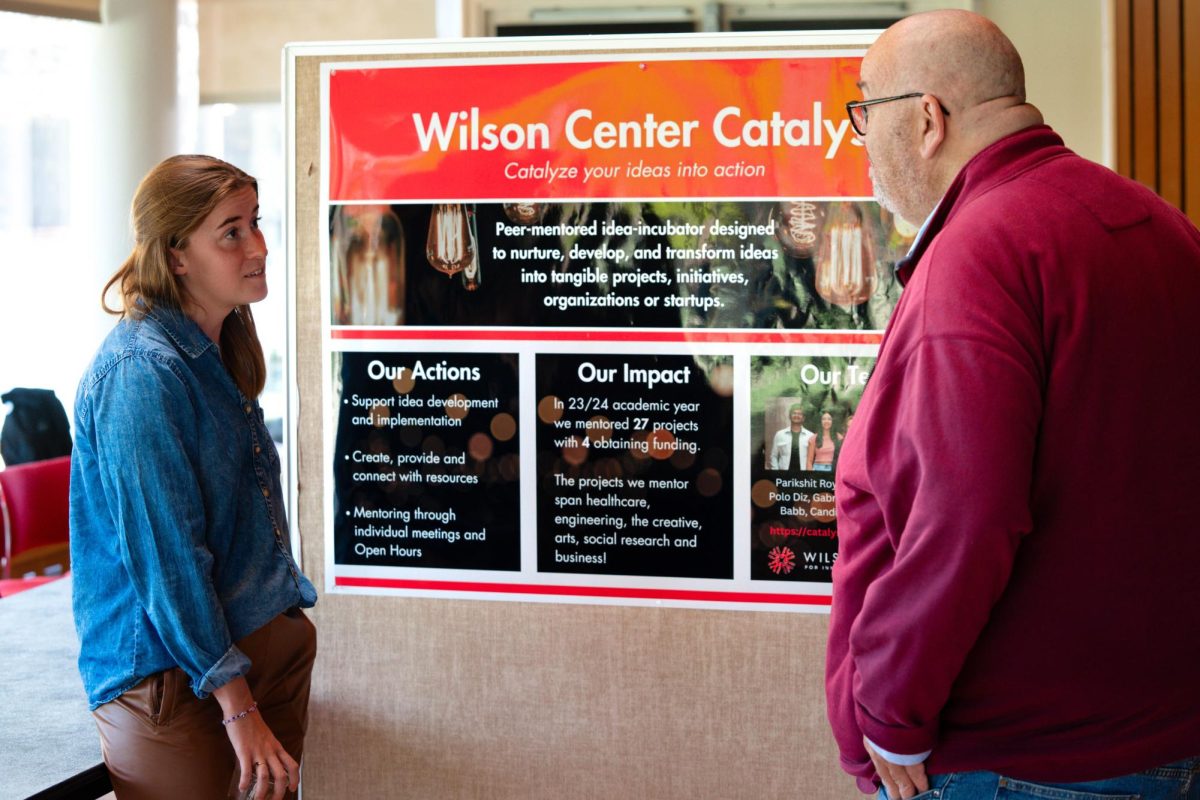
Advocacy is usually thought of as large-scale projects like sharing stories and gaining publicity for an issue to initiate systemic change, but advocacy work doesn’t always have to be big or flashy. I think of advocacy as authenticity: openly sharing your story and the values that stem from it, and not being afraid to start hard conversations with peers, providers or other community members.
While I participate in advocacy on the local, state and federal levels, speaking up for myself and initiating conversations in my personal life has impacted me the most. For me, this mostly took place with providers, teachers and peers. Advocacy in the exam room created the most tangible change: receiving better care. After gaining the courage from support groups and patient advocates, I decided to tell health care providers when I thought they were missing something, emphasizing my symptoms and asserting that I knew my body better than they did. While this didn’t always bear the results I wanted, it made me feel just slightly more in control of my health and proved, above all, that I do know what’s best for myself.
Grinnell is a very different atmosphere than rural Nebraska, where I grew up: people here tend to be much more educated on issues involving different identities, disability included. I feel that it’s never been difficult to have conversations around accessibility, stereotypes and other key issues that affect the disabled community. This increased willingness to learn about, understand and accommodate various backgrounds and lived experiences has brought me a sense of comfort and allowed me to be more open regarding my social and academic needs. Accommodations are far more common here than they were in my high school, and Disability Services makes the process of navigating academics much easier.
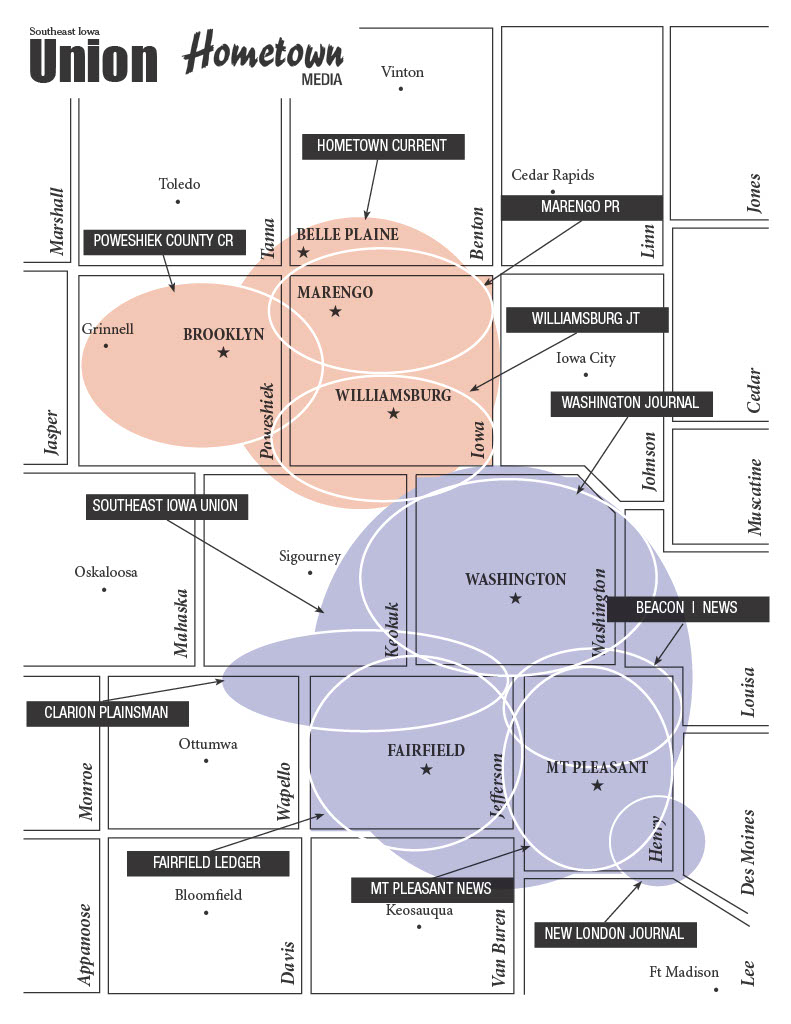
In my experience at Grinnell, accommodations are much easier to attain and people are much more receptive to social issues regarding disabilities, but there are still things that need to be considered on campus regarding health and wellness. When my health started to decline during the 2022 spring semester, I needed a series of appointments in Iowa City. For the several months that I was struggling, I felt as if I was drowning trying to coordinate appointments and procedures, take care of myself, keep up with my school work and maintain my social life. It was too much to juggle.
Following my first real experience trying to manage my health and academic load on campus, I realized how unattainable care is. You constantly have to choose between prioritizing your health, succeeding in your classes and having a life outside of school. Transportation to appointments is expensive, and despite having a hospital in town, specialty appointments require you to drive to either Des Moines or Iowa City. I’ve shifted my priorities because I don’t think that students should ever have to put their health on the back burner, and I don’t think that disabled students should be forced to fall behind or sacrifice their mental health to take care of themselves.
I’ve shifted my priorities because I don’t think that students should ever have to put their health on the back burner, and I don’t think that disabled students should be forced to fall behind or sacrifice their mental health to take care of themselves.
This month is Dysautonomia Awareness Month, one of the awareness campaigns nearest to my heart. It is particularly pertinent considering that around two-thirds of long COVID-19 patients develop Dysautonomia. In my work moderating support groups for Dysautonomia International, I have found the support groups flooded with long COVID patients. While the statistics aren’t clear, a recent CDC analysis suggests that around one in five people infected with COVID-19 will experience long COVID symptoms, which equates to almost 20 million people in the U.S. alone. These patients don’t have clear treatment regimens, many struggle to maintain the life they had before COVID and to make matters worse, they don’t qualify for disability benefits. While some interventions have been attempted, most notably Senator Tim Kaine’s attempted long COVID bill, nothing has been done yet, and millions of people are falling through the cracks of the U.S. healthcare system.
There’s a lot more advocacy to be done to continue to make sure that patients are being taken seriously, make a space for patients to share their stories and ultimately ensure that patients are able to receive support and an invaluable sense of community during a difficult time. Since the pandemic, addressing serious concerns about healthcare has entered the national dialogue, but I still believe that there is more work that needs to be done. While we can’t individually reform the healthcare system, we can take control of our own health by prioritizing caring for ourselves and giving our bodies the respect they deserve. My experience has taught me to always advocate for myself and my needs, and I hope it can help you do the same.