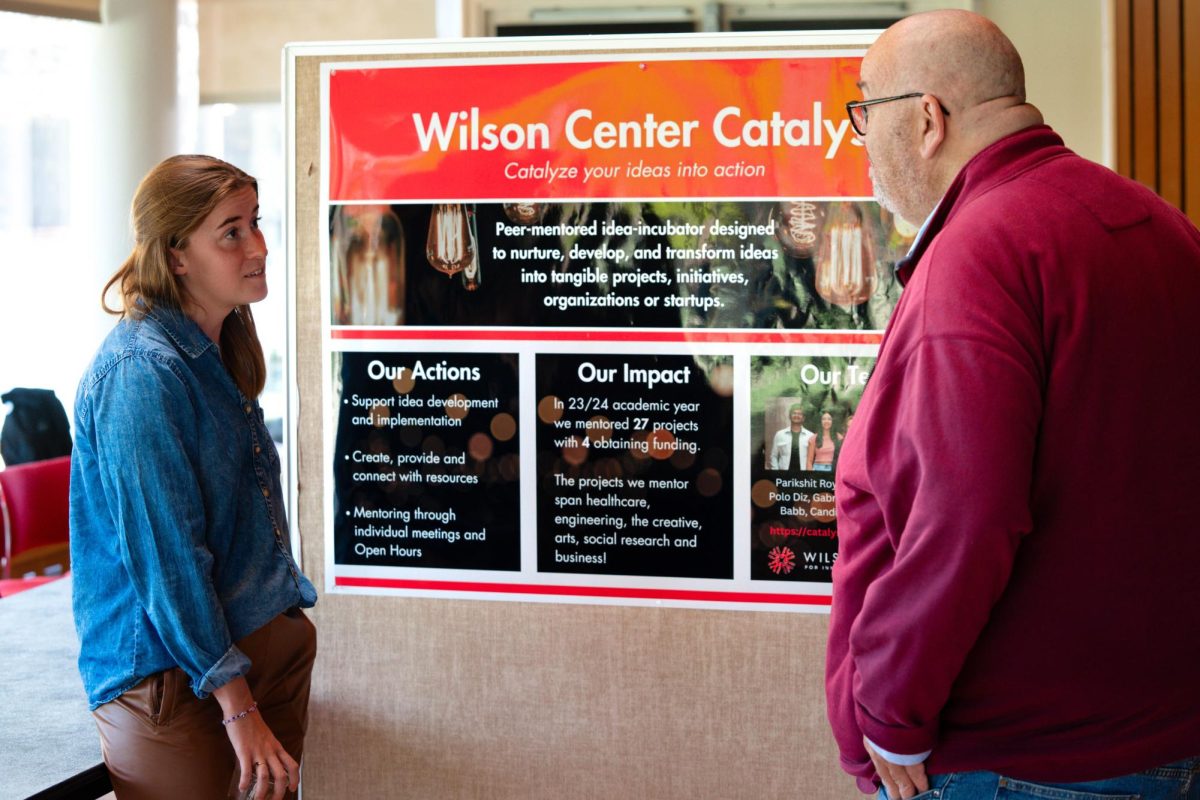
Dr. Craig Henderson ’63 has been one of the leading experts on breast cancer for the last two decades. Henderson started practicing medicine in the mid-1970s and has continued to treat patients in addition to being a teacher, researcher and, starting in 1995, a CEO of SEQUUS Pharmaceuticals. He left SEQUUS in 2001 and founded a new biotechnology company, Access Oncology, Inc. Henderson has also worked with the Food and Drug Administration and currently serves on Blue Cross/Blue Shield’s Medical Advisory Panel. Henderson has been a trustee at Grinnell since 2000 and taught a short course entitled From Bench to Bedside: Developing a New Anti-Cancer Drug this fall. On Wednesday afternoon, he spoke about health care policy in America, focusing on the work that advisory panels like MAP do.
How did your education at Grinnell shape your interests? How does it still change you today?
If you’d listened tonight, you’d hear someone who was being very critical of all the evidence. I really learned that skill set at Grinnell. That’s what I think you learn better at Grinnell than anything else. Grinnellians—whether they’re on the artsy side or the sciency side, the top of the class or the bottom—do this well. I call that critical thinking.
We actually discourage critical thinking at professional schools. Ph.D. programs may be different, but maybe not. You do have to create something. At the beginning, you’re just overwhelmed with learning, so you just want easy rules. I remember I had a resident who created these little cards called Bragg’s Laws, like an amp [small unit of measurement] of anything never hurts. Another one was if the patient’s in arrest, you’ve got nowhere to go but up. Patient’s still not breathing, tongue’s out, banging on their chest, you just try an amp of this, an amp of that. I mean it’s that kind of thinking simplicity that gets you started, but a lot of doctors never go beyond that, and I think it would be harder for a Grinnellian not to go beyond that.
There’s always this sense of discovery, too. You said during the presentation that you consider yourself kind of a hardass.
Well, first of all, I didn’t plan to go into cancer. That was a fluke. I wanted to avoid cancer, all those dying patients, remembering all those names of cancer types. I didn’t like it, I just thought I’d skip it. It’s kind of biology, like where you learn those [taxonomies], where you classify all the plants and animals and so on. That’s what cancer was when I was in medical school.
So I went into the lab in my third year, and then finally got really turned on by it, so I went to the cancer institute. They had all the money and the best labs. So I went down there, and I realized that my patients were dying every day and part of it was the crap that we were giving them. You say, we’ve gotta find something better than this. And what keeps you together is testing things that are new and different, because you know that they’re going to die anyway and the stuff you’re giving them has these terrible side effects. You’re happy to have some new drug to try, some new approach, and that comes from the critical mind.
How does seeing patients inform your research in general?
I still see patients to this day. The thing about it is that it really keeps you focused. I mean, I spent a lot of time learning to be a doctor, and a lot of time learning to be a breast doctor, and I don’t want to lose it. I mean, I get paid by the university and it’s all pro bono for me, but nonetheless I continue to do it because it lets me know what’s important and what’s not. Patients asked good questions, too.
Have they ever directly stimulated your research?
Over and over. Multiple times. It’s out of patient’s questions that you go directions you never would have gone before, or it’s the dilemma that they bring up, that they maybe can’t articulate. I try to figure out what’s right for that patient and realize there’s no evidence, I just have to go by what I intuitively believe.
Well it sounds like you have a lot of problems with the American medical system, as you went through your presentation. What do you think the main issue is?
The biggest single problem in American medicine is fee for service. You know, I came back to Iowa for Reunion and one of my best friends from high school, who’d nurse-trained at Mayo clinic, and I immediately started talking on the health care stuff. And she started on how she wasn’t going to live in a system where we have an “English” healthcare system. How can this woman, highly educated, who works in our system, think that this has anything to do with health care delivery at all? All we’re saying is that we’ve got to pay it, and we’ve got to figure out how to get the money to pay for it. That doesn’t have to be done by the government. I share her lack of enthusiasm in the government, but I think we have to get rid of fee for service.
In any kind of situation in life, you want to align your incentives with what you want as an outcome. So you say you don’t want an excess number of tests, we don’t want an excess number of procedures that don’t work. But that’s what we pay for! I’ve had a charmed career, and I’ve always been salaried and I’ve never actually had to charge a patient a fee for a visit, never. Never had to, never will. I get a little cranky if people interfere with what I want to do. And so people left me alone, because I get enough visibility that I was bringing patients in.
So my initial visit with a patient is never less than two hours. Sometimes it’s three hours, sometimes four hours. And afterwards the patient is leaving and says: “This was so wonderful! Why doesn’t everyone do this?” I say: “Well, if you paid them for the time, they would do it.” But you’re not willing to pay for the time.
In fact most patients…even ones who have been billed after meeting with me are often very frustrated by it, even though the three or four hours might be $300-400 and having some tube put up their tail or to have something put down their throat or have something cut out might be $5000, and they wouldn’t think about it.
Somehow I feel like knowledge, and the interaction we get, should be free. If you paid people for their time, and for their knowledge, you’d be amazed at the benefits. We’re getting what we pay for, and we ask for lots of new drugs and lots of new tests and that’s what we’re getting.
It sounds like you’re advocating for maybe something like a more holistic approach to medicine.
Well no. Well yes. Ok, so almost all of my patients have psychological problems, and if you had cancer and were facing death, you would probably have them, too. So do I need to send them all to a shrink? No, I’m a cancer doctor. I should be taking care of those. Now some of them are going to be too severe, like if they need Lithium for a bipolar disorder, which is exacerbated by cancer, then I’ll get a shrink in. But for most of them I should be able to take care of them. After all, every doctor is trained in psychiatric disorders, it’s part of your medical training. So in that sense, yeah, more holistic.
Do you think this sort of training should be emphasized more in medical school?
Yeah. But it’s not very sexy. I mean think about the things you’re interested in at 25 or 18 are very different than the things you’re interested in when you’re 50 or 60. It’s the way it is. I’m not so certain that “train” is all that important. You have to learn a certain amount of things the hard way. Now I won’t say it’s unimportant.
For example, when I was medical student, we used Kübler-Ross. She was one of the first people to write books on death and dying, and she was a nurse and a nun, I believe. She talked about the stages of dying, and she kind of systemized it. Now I think there were a lot of things, as I got more experienced, that were wrong in her story, but it enabled me to ask questions and think about it, and so in that sense it was good.
On the other hand, you can’t take someone who’s intrinsically insensitive and who never listens and turn them into a sensitive doctor with training. Sometimes patients will ask “Doc, why did you do this like this?” And I’ll say “Because my mother trained me to do it like that. It wasn’t something I learned in medical school.” My mother’s been very important in how I practice medicine. You can’t leave Grinnell after four years without examining your values seriously. It’s an intrinsic part of what’s Grinnell.
Trustee Henderson speaks on health care policy
November 6, 2009