It’s time to talk about eating disorders
February 20, 2023
CW: In this series, I will be discussing eating disorders and their devastating effects. As someone who has an eating disorder, I try my very best to never describe specific behaviors or numbers as that can be very damaging, but the material may be upsetting nonetheless. If you decide not to read, thank you for taking care of yourself.
Eating disorders aren’t uncommon, but in the throes of my relapse during my first year of college, they weren’t talked about by coaches, faculty, or really any of my teammates. The topic felt taboo. I was slowly killing myself (something I will get more into later), and felt deeply alone. When I finally reached the point of wanting help, I had trouble finding resources. I didn’t know who to talk to, and since no one talked about the issue, it felt far too daunting to bring it up myself.
So, six months into my recovery, when I returned to campus, I vowed to be candid about my disorder and recovery journey because I knew the difference it would have made for me if others had talked about their experiences. I wanted others to know that recovery is possible because I didn’t used to think it was. For most of my life I felt deeply ashamed of my disorder, but in learning about my illness, I realized I didn’t have control over what happened to me. I wasn’t going to judge myself, and if others judged me, so be it.
When I was in residential treatment the fall of my second year, the staff of dieticians, therapists, psychiatrists and doctors agreed that it is impossible to recover from an eating disorder while still engaging in disordered behaviors, and unfortunately, excessive exercise was one of my biggest behaviors. Much to my chagrin, no one at my treatment program really cared about my cross country career — they were more concerned with keeping me alive. So, my new 20-minutes-twice-a-week cap on exercise reduced my mileage to just 13% of my typical mileage while in season, and competition was off limits (competition is a huge part of exercise and something I will talk about in my next article).
When school resumed after the pandemic in fall 2021, I considered quitting. I couldn’t run and I didn’t know half my teammates, but being a cross country runner had been such a core part of my identity for so long — my team, my home — so I decided to stay. My coach offered me a managerial position, but I didn’t want that role. My situation felt more akin to an injury, so when people asked me if I was injured, I told them yes, I had an eating disorder. When they stared back at me blankly, I furthered my explanation: “my brain is very injured and it needs time to heal.”
In my pursuit to normalize recovery, I spoke more casually about my eating disorder, and found that I was filling a void on campus — people both in and outside of the athletic department came to me for support. “I’m worried my friend has an eating disorder. What should I do?” “I have an eating disorder, but I don’t want to leave school.” “You are the only one who understands. Can we talk?”
While I was always happy to chat and lend help where I could, I simply do not have the tools or resources to adequately support these individuals. In some cases, I was the only person who knew about their disorder. Time and time again, I have seen coaches, families and friends fail to provide resources, treatment and care to those who desperately need support.
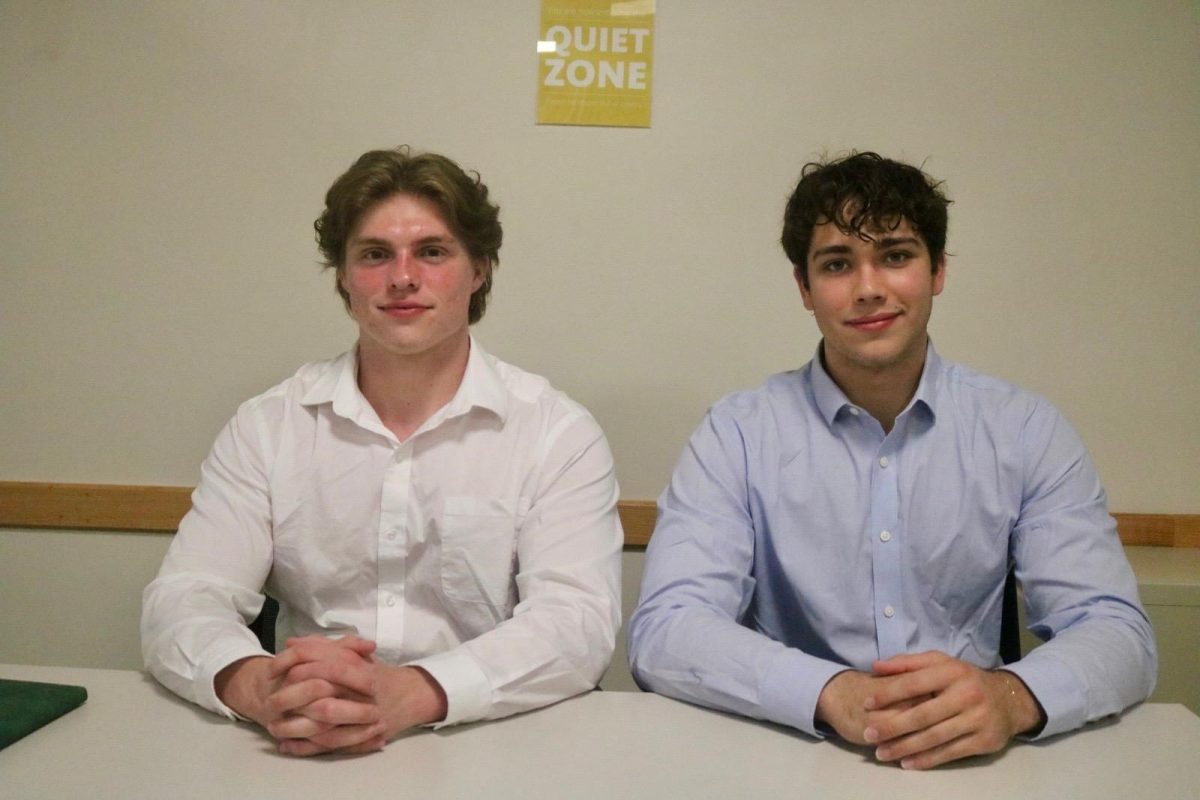
I’ve written about mental health in my column Mental Musings published in the S&B for years, but I always struggled to talk about eating disorders. They are an extremely nuanced and often very misunderstood topic, and I am terrified of misrepresenting anyone’s individual experience. However, nothing in my life has ever felt so pressing or important, so over a year ago, I began interviewing dozens of athletes, coaches, trainers, Student Athlete Mentors and faculty to gain more knowledge about how eating disorders are addressed at Grinnell College. I do not pretend to be the only person on campus who is aware of or trying to do something about this issue — there are many people who deeply care. One name that came up a lot in interviews was Carissa Tigges, the head athletic trainer and someone who many Grinnell teams use as a resource for eating disorder care. When I spoke with her last spring about writing this article, I told her about my experiences and impetus for interviewing her, and she responded, “We’ve had a handful of athletes that have gone to inpatient treatment, but you are the first one I’ve heard that would say it out loud.”
Tigges is one of many to comment on my candor. It is rare to hear someone talk about an eating disorder diagnosis, and many tell me I’m the first person they’ve heard talk about it openly. Our society has made leaps and bounds when it comes to discussing mental illness, yet eating disorders remain severely stigmatized.
The absence of substantive dialogue leaves both those with eating disorders and those trying to support people with eating disorders with an alarming dearth of information. This lack, combined with an utter scarcity of resources, has led me to believe that people with eating disorders may be one of the most under-supported groups on campus.
This disease is too common and too dangerous to ignore. Eating disorders have the highest mortality rate of any mental illness; the it has been estimated that someone dies from eating disorder complications every fifty-two minutes. Heart attacks, dehydration, electrolyte imbalance and other physical complications often lead to death, but suicide rises to the top as the number one cause of death for those suffering with an eating disorder. The Center for Discovery states that having an eating disorder makes a person 32 times more likely to attempt suicide, and that up to 20% of all untreated cases of eating disorders end in suicide.
I use the term eating disorder a lot, so I feel that it would be good to discuss what that means. Most of us first conjure up an image of an extremely underweight individual who goes to extreme measures to reduce caloric intake. While not inherently wrong, this depiction is only true some of the time. Although the behavioral and physical aspects are the most talked about components of an eating disorder, in reality, that definition barely scratches the surface. Every health professional I interviewed said that eating disorders are first and foremost a psychological phenomena. In an article for ATTN, Dr. Rebecca Wagner, director of the Eating Recovery Center, argues that eating disorders completely take over people’s lives, affecting their relationships and ability to function at work or at school. In other words, over time, the disease deprives people of everything that is important to them.
That doesn’t mean that eating disorders aren’t or can’t be physical. From damage to eyesight and decreases in bone density to irregular heartbeats and lessened brain functioning, eating disorders indeed also pose very serious threats to our physical health.
Eating disorders, like most mental illnesses, exist on a spectrum. Many people have a fraught relationship with food and/or their bodies without having a diagnosable eating disorder. Given current diet culture and impossible beauty standards, it can be hard to tell when someone is in need of help. They can affect people of all ages and demographics, but the most common ages of onset are 14 and 18. Therefore, early intervention is crucial because eating disorders become more severe and less receptive to treatment over time.
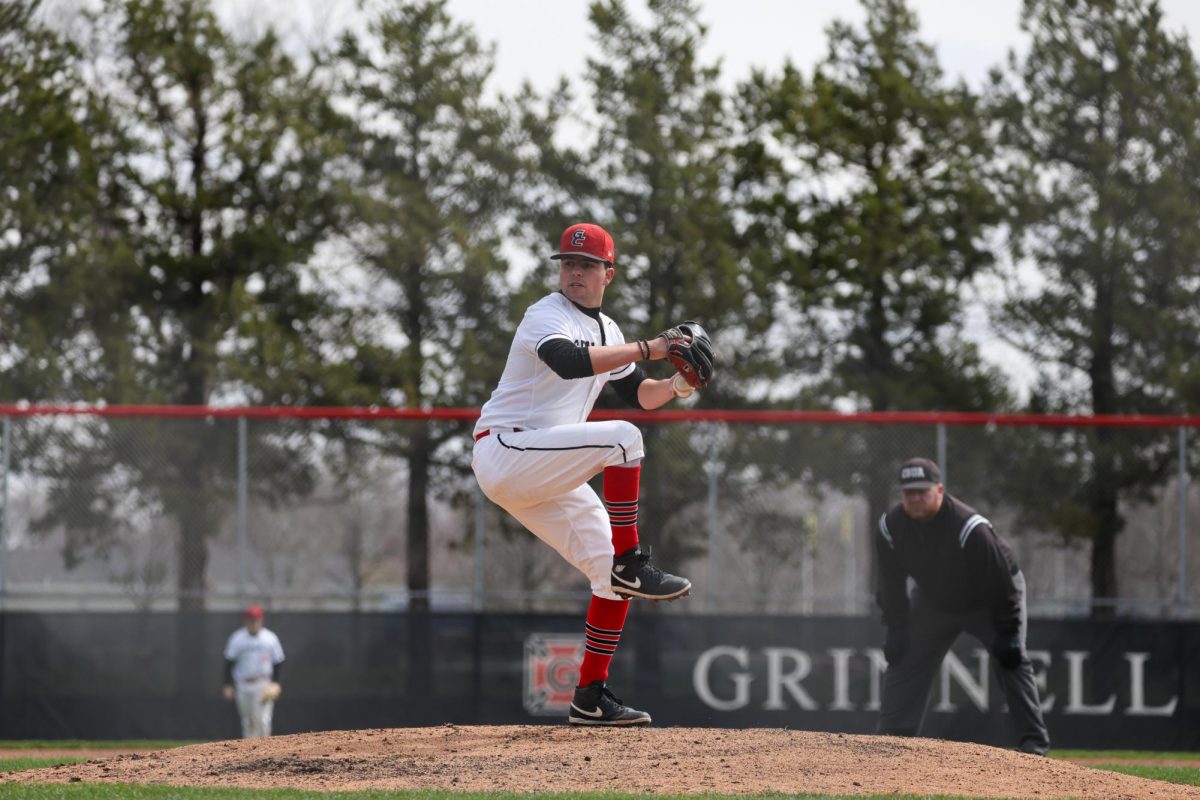
I focused this series on athletes because athletes represent the population at the highest risk. Psychologists from the University of Utah and Tulsa University separately both estimated that one-third of female collegiate athletes suffer from some kind of disordered eating. While female endurance athletes top the charts for rates of disordered eating, all athletes are at higher risk for disordered behaviors. One particularly salient example from Newsweek reported that 40% of Cornell University’s football team participated in binging and purging.
Many people in the Grinnell athletics department and on campus are aware of this issue. When I spoke with Birant Akbay, a doctoral psychology student at the University of Iowa who sees students at Grinnell and hosts athlete support groups, he said, “We just don’t have that resource yet. But, it doesn’t mean that coaches aren’t aware that there’s a gap in those resources and SHAW isn’t aware. They are aware. I think they’re at least starting to push for change.”
The stigma surrounding eating disorders, coupled with a serious lack of resources, has left us in what I consider a crisis. During my interviews for this series, some of the people I talked to — the professionals and people in charge, the people a person struggling with an eating disorder might go to for support — began taking notes, asking me for resources or to share the research I had done or speak more about my experiences. Our conversation turned into more of a brainstorming session, as both of us tried to figure out how to help current students.
Change is possible. We can provide people who are struggling with eating disorders the support, but we first need to break down the stigma and misconceptions and prioritize creating more resources on campus. I talked with many individuals across campus who offered their stories and suggestions, and in future articles I hope to provide my insights on the next steps of how to get there.